Did you know that our very own Dr. Benjamin Barankin was recently published in The American Journal of Clinical Dermatology discussing Acne and Acne Scarring.
Did you know that our very own Dr. Benjamin Barankin was recently published in The American Journal of Clinical Dermatology discussing Acne and Acne Scarring.

Em Ford is a globally recognized acne activist, YouTuber, and powerhouse behind the #SkinPositivity movement. The 29-year-old British vlogger and activist uses her YouTube channel, My Pale Skin, as a platform to empower women with the confidence to live their lives without the fear of being judged for their appearance.
For “Teen Vogue,” Em shares a list of the things she wishes people knew about dealing with acne.
1. Your Skin Doesn’t Define You
I’ve accepted that some days are going to be harder than others. Some days I will wake up and be comfortable in my skin — there’s been no-flare ups, breakouts or soreness, it’s a mild day — and I’ll instantly feel more confident because of this. Other days, if I have a major breakout, I’ll just want to hide because I’m worried about what other people will think and say. But I’m more than my skin on a good day and a bad day; your skin does not define you as a person.
2. You Need the Patience of a Saint
It’s been an ongoing battle for years of my life, and it takes up a lot of time. It’s so easy to lose patience with your acne, and lose track of what’s important. I know some days will feel harder than others, but you have to learn to love the person you see looking back at you when you look in the mirror. Rather than focusing all of your attention on the things that you don’t like, embrace all of the things that you do! It isn’t going to happen overnight, but once you begin to love yourself you will feel so much happier in yourself.
3. It Can Impact Your Social Life
Acne can impact so many aspects of our lives, and I would often cancel plans and avoid social situations because I was self-conscious that people would notice my skin before they noticed me, especially if my skin was particularly bad that day. I was convinced that people couldn’t see past my acne and I couldn’t go out and enjoy myself because they would be focused on my flare-up, bad blemishes; even just general glances felt like hate. So I stayed in. But don’t let them win. Stay strong. And if you’re reading this and you can see this happening to a friend, reach out, check in, and be there.
4. There Is No Magical Cure
Unfortunately, as many skin-care experts will tell you, there is no one size fits all for acne treatments. Everybody is different. I’ve spent so much money on products and treatments that have been recommended to me by others because it has helped their skin, but made my skin break out even more. It takes time to find what’s right for you and your skin.
5. Find What’s Right for You
Don’t get discouraged when things don’t work right away. Before spending a lot of money on expensive treatments, I recommend booking an appointment with a dermatologist who can sit down and talk you through some of the best options that could work for you.
6. You’re Going to Want to Pick, But Don’t
The temptation can be overwhelming, but picking at your acne is one of the worst things you can do, and your skin is going to pay for it. Flare-ups might seem bad, but the scarring that is left behind is often worse, because the skin on your face takes a long time to heal. Picking can cause permanent scars, and red marks that are hard to get rid of.
7. You’re Not Alone
Receiving thousands of extremely kind and personal messages from people on social media has really helped me get through my worst days. Knowing that the feelings and emotions I experience daily because of my acne are felt by so many others is the reason why I wanted to open up about it. The confidence I’ve gained through sharing my experiences and hearing about my followers’ experiences is what I hope to bring to others. We’re all in this together. Just take a look at the #SkinPositivity hashtag, where you’ll find a community of people waiting to embrace you.
8. Be Mindful of Everyone’s Journey
In 2015, when I decided to open up and share my story on social media with #YouLookDisgusting, showing the real me in makeup-free images, my life changed in ways I couldn’t have imagined. My content was being viewed by millions of people around the world, but the negative comments that came with that weren’t something I could prepare myself for. In the beginning, I found this really hard to deal with and the negativity definitely got to me. What enabled me to carry on was the support and messages I received from thousands of others who were going through similar struggles, who reached out to me and let me know that my videos made them feel less alone on their journey.
9. We Don’t Feel Represented
Social media and some beauty brands put out a stigma that you shouldn’t have bad skin and those that do need to fix it. If only it were this easy. Someone who suffers with acne shouldn’t be made to feel any less beautiful than people who don’t. Beauty comes from the inside out. We need more brands across the beauty, fashion, and lifestyle spectrum to change the way they look at acne and promote the message: It’s okay not to be perfect. I’d love to see a campaign with women who don’t have perfectly airbrushed skin. We’re owed it.
10. There Is Nothing Wrong With You
No matter your age, moment in your life, or time of day, acne is one of the most common skin conditions. It’s natural. There’s nothing wrong with you. It can feel like the worst thing in the world, but you’ll find your way to own it.
Credit: Em Ford, teenvogue.com
Lasers are an important component of a cosmetic medical practice. They treat many skin conditions, such as hyperpigmentation, acne, telangiectasia (blood vessels), aging skin and many other conditions that are not easily treated by typical facial treatments. Patient education on pre- and post-laser care will optimize results and increase the patient’s satisfaction with their provider and their finished look.
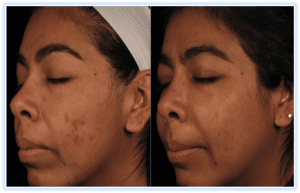 Patients with pigmentation disorders, such as solar lentigo, photo/sun damage, post-inflammatory hyperpigmentation and melasma, can achieve significantly better results if they take care of their skin at home. Most pigment disorders can be treated easily with visible light laser or intense pulsed light (IPL or BBL), except in the case of melasma. There has been success treating melasma with fractionated erbium laser treatments and other modalities, and several treatments are typically needed.
Patients with pigmentation disorders, such as solar lentigo, photo/sun damage, post-inflammatory hyperpigmentation and melasma, can achieve significantly better results if they take care of their skin at home. Most pigment disorders can be treated easily with visible light laser or intense pulsed light (IPL or BBL), except in the case of melasma. There has been success treating melasma with fractionated erbium laser treatments and other modalities, and several treatments are typically needed.
When treating patients with pigment disorders, home care is critical. Topical agents containing pigment-lighteners should be used at home for four to six weeks before treatment with continued use until the desired outcome is reached. Some popular pigment-lightening ingredients include hydroquinone, which many professionals consider to be the most effective pigment-lightener on the market. If a patient develops sensitivity or is looking for alternative treatments, the ingredients kojic acid, ascorbic acid (vitamin C), azelaic acid, licorice root and arbutin, as well as many others, can be used with good, although slower results. These ingredients work by suppressing the activity of the melanocytes, which are the cells in the skin that produce pigmentation to protect it from irritation, inflammation, acne, hormonal conditions and photo damage. Those with darker skin have more active melanocytes; therefore it is an absolute necessity to pre-treat darker skin types so the risk of complications is decreased. Along with pigment-lighteners, sunscreen is an absolute must. If the proper sunscreen is not used before and after treatments, patients increase their chances of undoing the results they have obtained or increasing their existing pigmentation.
 For patients with rosacea or vascular issues, IPL or BBL, or visible light lasers are the most effective treatments. Light therapies are attracted to color and cannot differentiate between tanned skin and target colors; therefore, patients must use a topical high-quality broad-spectrum sunscreen before and after treatments. Zinc oxide is often preferred because it is a physical sunscreen with anti-inflammatory properties. Topical vitamin C and vitamin K could also be used to achieve favorable results. Vitamin K decreases the pooling of blood under the skin commonly associated with telangiectasia, and vitamin C has been shown to strengthen capillary walls, therefore decreasing the chances of further damage. Care for these patients is simple compared to other skin conditions that are treated with lasers. Always remember, less is more with these skin types. It is imperative to educate the patient about the importance of wearing sunscreen on a daily basis and about ways to avoid further damage. The patient should also be aware of triggers that will cause breakouts.
For patients with rosacea or vascular issues, IPL or BBL, or visible light lasers are the most effective treatments. Light therapies are attracted to color and cannot differentiate between tanned skin and target colors; therefore, patients must use a topical high-quality broad-spectrum sunscreen before and after treatments. Zinc oxide is often preferred because it is a physical sunscreen with anti-inflammatory properties. Topical vitamin C and vitamin K could also be used to achieve favorable results. Vitamin K decreases the pooling of blood under the skin commonly associated with telangiectasia, and vitamin C has been shown to strengthen capillary walls, therefore decreasing the chances of further damage. Care for these patients is simple compared to other skin conditions that are treated with lasers. Always remember, less is more with these skin types. It is imperative to educate the patient about the importance of wearing sunscreen on a daily basis and about ways to avoid further damage. The patient should also be aware of triggers that will cause breakouts.
Mature skin that is characterized by fine lines, wrinkles or increased laxity benefit most from ablative laser treatments. One of the most popular and effective treatments available today is the fractionated Profractional laser. Care for the patient’s skin after treatment with the Profractional laser is critical, because it can affect the healing process and the results. Patients with darker skin should be prepped with pigment-lighteners before and after these treatments in order to prevent the possibility of adverse reactions, such as hypopigmentation and hyperpigmentation. The patient must also be taught the importance of keeping the skin occluded with an ointment recommended by the treating physician. Along with a gentle cleanser, this ointment is the only product that should be used for the first two days following a deep ablative laser treatment.
The main purpose of these treatments is to create a wound response in the skin so more collagen will be produced. If the skin doesn’t have a healthy environment to generate this collagen, patients may not achieve optimal results and it can increase the likelihood of complications. The skin heals best in a moist environment; therefore, after the initial healing period, hydrating agents including hyaluronic acid and emollient moisturizers should be used. Peptide-rich products may also be applied to aid in the healing process.
 Lasers may also be used in the treatment of acne, which occurs because oil glands are stimulated to produce more sebum. In addition to this overproduction of sebum, dead skin cells accumulate in the excess oil. This excess buildup of skin cells and oil acts as a breeding ground for Propionibacterium acnes, which is the bacterium that worsens acne. Laser light in the red to blue spectrum may be effective at killing this bacteria and decreasing the inflammation associated with it. The laser works not by heat, but by activating a protein to destroy P. acnes and the surrounding inflamed acne lesions. Lasers alone or photodynamic therapy, a process where lasers are used in conjunction with a topically applied solution, have proven highly successful. Photodynamic therapy utilizes a topical drug called Metvix to photosensitize the P. acnes bacteria, making them more susceptible to laser light. Proper product use during this treatment is essential. Gentle cleansers, sunscreens containing zinc oxide and hydrating agents, such as hyaluronic acid and vitamin B-5, should be used.
Lasers may also be used in the treatment of acne, which occurs because oil glands are stimulated to produce more sebum. In addition to this overproduction of sebum, dead skin cells accumulate in the excess oil. This excess buildup of skin cells and oil acts as a breeding ground for Propionibacterium acnes, which is the bacterium that worsens acne. Laser light in the red to blue spectrum may be effective at killing this bacteria and decreasing the inflammation associated with it. The laser works not by heat, but by activating a protein to destroy P. acnes and the surrounding inflamed acne lesions. Lasers alone or photodynamic therapy, a process where lasers are used in conjunction with a topically applied solution, have proven highly successful. Photodynamic therapy utilizes a topical drug called Metvix to photosensitize the P. acnes bacteria, making them more susceptible to laser light. Proper product use during this treatment is essential. Gentle cleansers, sunscreens containing zinc oxide and hydrating agents, such as hyaluronic acid and vitamin B-5, should be used.
It is important to not only have the patient’s skin prepped properly, but also to care for the skin after these treatments. Along with any medical treatment, using the wrong products will not only hinder the results, but can also cause serious complications. Education is the key to achieve the best outcome, and the ultimate gratification comes when satisfied patients obtain great results.
~ Sheri Roselle, Medical Esthetician at Toronto Dermatology Centre
 U of A dermatologist says most people know the risks, but still get caught out.
U of A dermatologist says most people know the risks, but still get caught out.When University of Alberta dermatologist Robert Gniadecki was growing up in Denmark, getting a sunburn was part of every family holiday.
“The first day at the seaside you would go out in the sunshine, and the next day you would have a bonfire, peel your skin off and throw it in the fire,” he said.
“It’s so disgusting, when you think about it today, but 40 years ago this was a normal thing.”
Gniadecki said these days most of us know that even a tan is a sign of skin cell damage, but sunburn still sneaks up on us from time to time. He shared four surprising ways people can get burned:
Foods that increase your UV sensitivity
Turns out “margarita sunburn” isn’t just a reference to what happens when snowbirds roast on Mexican beaches. There’s a naturally occurring chemical called furocoumarin in limes, some kinds of carrots, celery, dill and other plants that, when ingested, causes your skin to become more sensitive to the sun’s harmful rays.
“And of course people often fall asleep after having a couple of drinks, which doesn’t help either,” said Gniadecki. “A simple thing like sleeping in the sun is terribly dangerous.”
Unexpected weather changes
It even happens to dermatologists.
“I was on a rainy winter hike in the mountains,” Gniadecki said. “Then the clouds cleared and I was left on a snow patch with no protection.”
More UV than you realized
Most of us realize the sun’s rays are stronger at the equator than in our own backyard, and weaker at sunset than at high noon—it’s all about the angle of the sun. What we may not realize is how ultraviolet light is concentrated when we are on water, sand or even snow.
“People often think that in winter, because it’s cold and you don’t feel the warmth of the sun, you will never get a sunburn or you can tolerate more sun,” Gniadecki said. “You can actually tolerate less sun during the winter because of the reflection from the snow.”
He said that sun exposure is almost doubled in the snow, compared with being on grass, while sand reflects 15 to 20 per cent more and seawater reflects 25 per cent more UV than grass.
Sunscreen spread too thinly
Gniadecki said you need to apply enough sunscreen to create a sheen all over your skin. If you’re using sunscreen that contains titanium or zinc oxide, a white hue should be visible. Be sure to use a product with a sun protection factor (SPF) of at least 20, which lets through just 1/20th of the sun’s harmful rays. That means that if you would normally start to burn in 10 minutes, you can stay out in the sun for 200 minutes. But be realistic about how long your exposure will be, and reapply your sunscreen if you get wet.
“If you sweat a lot, some will wash away, and you can get a sunburn,” said Gniadecki.
He recommended avoiding sunscreens that contain oxybenzone, a common ingredient that was recently shown to be absorbed through the skin into the bloodstream. Gniadecki suggested using other products until the health effects of oxybenzone are better known.
Gniadecki recommends staying away from household remedies—such as applying cooking oil or yogurt, or the Danish prescription of putting lemon slices on your skin—which are not only ineffective, but could also be harmful. He suggests the following steps instead:
“The short-term effects of sunburn are trivial and you can usually manage them at home,” said Gniadecki, who is also a member of the Cancer Research Institute of Northern Alberta. “But the long-term effects are serious.”
Sunburn, especially in childhood, causes permanent and irreparable damage to the skin that can develop into cancer 20 or 30 years later.
“The skin will remember forever,” said Gniadecki.
Credit: Gillian Rutherford, folio.ca

Are you sure that that mole isn’t melanoma? According to the American Academy of Dermatology, one in five Americans will develop skin cancer in their lifetime, and one in 50 Americans will develop the life-threatening type of skin cancer, melanoma. While you can take steps to reduce the risk of skin cancer by avoiding excessive ultraviolet light exposure form the sun and tanning beds, early detection is critical to minimize the damage of skin cancer.
Most forms of skin cancer, even melanoma, are almost 100 percent curable if caught in the earliest stages of growth. That is why I routinely talk to patients about performing monthly self-skin exams. If a patient notices a growth that has been changing in size, shape, or color, I’ll want to see it right away to evaluate for cancerous changes.
So, how do you do a proper skin exam? Once a month, either getting into or out of the shower, spend a few minutes looking at your entire skin’s surface. A thorough skin exam does not have to take very long, but it require a long mirror and a hand-held mirror to really see everything.
It’s not practical or realistic to spend hours examining every growth on the skin. However, a good skin “look over” when performed on a regular basis will help you learn the pattern of all the moles, spots, lumps and bumps. The brain is very good at recognizing patterns and after a few monthly skin exams, should learn the general pattern of growths on the skin. If a new growth emerges, or an old growth becomes larger, people performing regular self-skin exams are more likely to notice the change to alert their dermatologist sooner.
Performing regular self-skin examinations are an easy way to take ownership of your skin health. I see men and women in the office all the time who notice a new little spot that “just doesn’t seem right, Doc.” In some cases, these growths were determined to be a very early melanoma. Early melanoma has a 99 percent cure rate, however, if allowed to spread, could have devastating consequences. So get out the mirror, and get to know your own skin.
Credit: Dr. Elizabeth Tanzi, washingtonian.com

This week a patient of mine told me that her nail girl told her to never have her underarms lasered because it causes breast cancer. Although I have often been asked if any radiation comes from our lasers (there is zero radiation from cosmetic lasers of any kind), I was curious as to where she got this false information. She said that the girl who does her nails knew a girl who had her underarms lasered and that person also had breast cancer.
The truth is that all cosmetic lasers, whether for hair removal, photo rejuvenation (e.g. IPL or BBL), skin resurfacing or anything else, has a wavelength in a safe zone, where there is no radiation emitted whatsoever. Each laser’s wavelength is attracted to a specific something, usually a colour. If it doesn’t see that colour, then it isn’t even absorbed into the skin. Yes, the skin, only the skin. In other words, the lasers can’t see the thyroid, the lymph nodes or any other part of the body that is more than skin deep. Dear nail girl: leave the facts to the professionals and keep your silly conclusions to yourself.
Here are some other myths about lasers:
The first dermal laser treatments were conducted by a dermatologist named Leon Goldman in 1962 for the removal of tattoos. Since then, cosmetic lasers have been successfully developed for the treatment of scars, varicose veins, birthmarks, wrinkles, hyperpigmentation, hair removal, and much more. There are thousands of clinical studies conducted on cosmetic lasers and their effective and safe use in many skin concerns has been proven many times over.
Laser treatments are developed through sound scientific principles to produce specific results while minimizing unwanted side effects. In hair removal treatments, for example, the energy from the laser is tuned to heat up and thereby deactivate hair follicles, thus preventing them from further activity. In the case of tattoo removal, the pigments in the tattoo ink are targeted, and the specific wavelength is designed to break up the pigments so they can be eliminated by the body’s waste systems. Provided a laser treatment is given within the specified guidelines and with the proper diagnosis of a trained expert, the results and side effects are almost always predictable and controllable.
Unlike store brand skin care products which may have all kinds of exorbitant claims, medical equipment such as cosmetic lasers are required by law to be thoroughly tested for effectiveness and safety. Laser machines cannot be marketed unless approved by the US FDA (or European equivalent CE mark) which sets stringent rules on claims that any equipment may make. For example, most hair removal lasers are not allowed to say that they give permanent hair removal, but only permanent hair reduction. This is because occasionally hair does regrow in an area after treatment, but it will be greatly reduced in quantity and appearance.
Skin care products on the other hand, are rarely required to prove their claims, so they can claim “better than Botox” or “as effective as laser” without repercussions. There are no skin creams or serums that can remove varicose veins, resurface and smooth out severe acne scars, reduce the appearance of birthmarks such as Port Wine Stains or help remove unwanted tattoos. Its simply not possible and doesn’t exist, nor will it ever.
Every single person is different, and what works for 90% of the population may just not be right for the remaining 10%. Depending on different factors such as your skin sensitivity, pain tolerance, or even your lifestyle habits such as smoking, excessive sun exposure or usage of certain drugs or skin care products, you may respond differently to a laser treatment. That is why it is important for you to trust your doctor, and allow him or her to determine the course of your treatment and deciding if you need to change the settings from your previous procedure or not.
Lasers do not cause the skin to become weak and thin, in fact the controlled heating and wound action of a laser treatment actually induces the natural skin reaction of collagen and elastin formation to replace the damaged skin. Even repeated usage of lasers will not cause the skin to be damaged or weakened, provided your laser provider has a thorough understanding of the limitations of the equipment he or she is applying to the skin.
Lasers are not a one size fits all, and most equipment is highly specialized and calibrated for specific purposes. There are two main types of lasers – namely ablative and non-ablative. Ablative or cutting lasers work by physically destroying the top layers of the skin, and are used in procedures such as laser resurfacing and scar revision.
Non-ablative lasers work by targeting specific depths or colors while leaving the top layer of the skin unharmed. Different laser modalities are calibrated for various uses including hair removal, skin rejuvenation, reducing excess pigment and tattoo removal. While a single machine can often be used to treat a range of different concerns, the wavelength and energy levels must be adjusted for each specific purpose.
Different laser machines are also calibrated differently and may have specific strengths, ie. Profractional laser is very good for acne scar revision and skin rejuvenation, but differs from the Cutera Excel V that targets hair and vein removal. Even rival hair removal lasers can differ in the skin / hair types which they are used for, so having a professional who knows the ins and outs of the equipment is essential for effective and safe treatment.
Fact: Lasers may be an established and well understood medical tool, but just like a kitchen knife has the potential to be deadly, a laser in the wrong hands has the potential for serious damage. A laser that is unreliable and poorly engineered or poorly maintained is even worse, which is why you need to ensure the laser equipment you are being treated with is safe.
Major medical laser names such as Cutera, Sciton, or Lumenis are continuously being tested for quality and safety as well as efficacy. The lesser brands that sell to spas don’t have equivalent parameters to follow and therefore don’t need to be as effective.
A laser treatment simply changes the conditions of your skin at the time of the treatment, and does not produce a dependency. For example, after an strong laser treatment such as a resurfacing procedure that vaporizes skin cells to encourage cell renewal, your skin will heal and become smoother, even, and more supple. You may need several treatments to achieve your end goal, but certainly there is no need to continually undergo treatments once you have solved the problems you wish to address. Eventually on-going aging and lifestyle factors will cause pigmentation, wrinkling or other problems to recur, which is when further treatments or a maintenance program may be necessary.
It is important to remember that a laser procedure is in fact a serious thing, and it is designed to cause controlled damage to induce the skin to heal and renew itself. A laser resurfacing procedure commonly produces a bronzing effect, as if you have had a sun burn, as the skin injury causes old and pigmented cells to die off and be replaced. Some swelling after the treatment may also be seen. Many doctors believe that although unpleasant, the more severe the reaction (tissue swelling, intense redness, flushing and sensation of heat), the better the results of the treatment. Other treatments such as hair removal may not produce as severe reactions, and any blistering or pus formation after a laser treatment is most certainly not desired. It is usually best to check with your physician or technician to determine if your post-laser reaction is indeed normal or if it needs attention, but bear in mind, a severe reaction is not necessarily a bad thing.
In conclusion, I wouldn’t ask my car mechanic how to do my plumbing, so it would only make sense to ask a professional in the required field of expertise that you are seeking answers for. Without the facts, you could be keeping yourself from achieving great results with cosmetic lasers that have proven themselves for many years to be safe and effective. When in doubt, ask your dermatologist or your laser technician. They are the ones who work with the machines and they are the ones who have the proper education to answer your questions based on facts and experience.
~ Sheri Roselle, Medical Esthetician at Toronto Dermatology

Negative emotions can trigger or worsen a wide range of conditions like acne, hair-thinning, and psoriasis.
Anxiety may originally arise in your brain, but the consequences can play out all over your face. And we don’t just mean a clenched jaw or a furrowed brow. Stress, anxiety, and similar emotional states can trigger or worsen a wide range of skin conditions, from acne to hair-thinning alopecia, to scaly psoriasis, research shows.
For instance, in one study of 101 people with psoriasis—an autoimmune condition that causes excess skin cells to build up in itchy, painful patches—about half reported that their first brush with the disease came during a particularly trying time in their lives. And about two-thirds said their symptoms worsened when they felt pressured.
Click here to read the full article.
Credit: vice.com

A 5-year-old girl was brought to the emergency room at Evelina London Children’s Hospital with itchy, rather unsightly sores on both legs. She had recently returned from a weekslong trip to Sierra Leone, and the lesions, which first appeared three weeks into her stay there, had become larger and ulcerated.
Diagnosis: cutaneous diphtheria, a disease rarely seen in many industrialized countries, including Britain and the United States, where most children are protected by the diphtheria toxoid vaccine, DTaP, and a booster shot of the tetanus-diphtheria-pertussis vaccine, Tdap.
Still, as more and more Americans of all ages travel abroad, often to less developed areas, travelers and doctors in this country need to be alert to unusual and often perplexing skin infections. Even though cutaneous diphtheria is not a notifiable disease here, between September 2015 and March 2018, four cases were reported to the Centers for Disease Control and Prevention.
The patients, two from Minnesota and one each from Washington and New Mexico, had recently returned from Somalia, Ethiopia and the Philippines, respectively.
The C.D.C. noted in its weekly report in March that reported cases of this highly contagious infection had recently increased 10-fold, from an average of only three a year during the period 1998 to 2011, to 33 a year during 2012 to 2017. Still, the agency said, these numbers underestimate the true incidence of such infections. Although the four new cases were confined to the skin, the lesions can be a source of a life-threatening respiratory infection in people not adequately immunized against diphtheria.
Thus, everyone who might have had close contact with the patients needed to be checked, perhaps treated with antibiotics, and if they lacked immunity to diphtheria, immunized with diphtheria toxoid-containing vaccine.
Read the full story on here.
Credit: nytimes.com
 With summer finally within reach, you’ll soon be able to find free sunscreen at select City of Toronto park locations starting this July.
With summer finally within reach, you’ll soon be able to find free sunscreen at select City of Toronto park locations starting this July.
The success of the #BeSunSafe program in waterfront parks last year has prompted the city to expand its public health program providing free sunscreen in select city parks this summer.
The Health Canada-approved SPF 30 broad-spectrum sunscreen will be available at 75 dispensers located in city parks along the waterfront as well as several new locations.
High Park, Riverdale Farm and Evergreen Brick Works dispensers have been added to this year’s program.
“Protecting and promoting good health is important all year, and especially during summer months. Making sure to apply sunscreen regularly, wearing sunglasses and seeking shade while spending time outdoors are great ways to stay sun-safe in warmer temperatures,” said Dr. Eileen de Villa, Toronto’s Medical Officer of Health.
“This initiative promotes positive health for our residents and visitors and I encourage everyone to enjoy summer activities while taking simple steps to protect themselves and reduce the risk of skin damage this time of year.”
Last year, 50 sunscreen dispensers helped to protect up to 94,000 Torontonians and raised awareness about preventing skin cancer. The 2018 program won the Canadian Dermatology Association Public Education Award.
A location map will be available online once dispensers are installed next month.
Credit: dailyhive.com